Online Course
Nurs 467 - Public Health Nursing
Module 8: Case Management, Screening, and Referral
DEFINITIONS
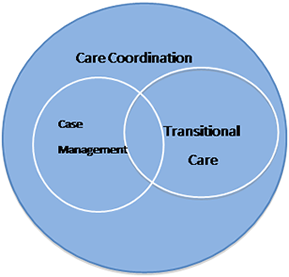
Care Coordination and Case Management - The Agency for Healthcare Quality and Research (AHQR, 2014) defines care coordination as:
The deliberate organization of patient care activities between two or more participants (including the patient) involved in the patient’s care to facilitate the appropriate delivery of health care services. Organizing care involves the marshalling of personnel and other resources needed to carry out all required patient care activities and is often managed by the exchange of information among participants responsible for different aspects of care.
Care coordination encompasses case management and transitional care management. While there is no universally accepted definition for case management. The Case Management Society of America (CSMA), a professional organization for case management, defines case management as “a collaborative process that assesses, plans, implements, coordinates, monitors and evaluates the options and services required to meet the client’s health and human services needs.” When done well, case management promotes good patient outcomes, effective interventions and efficient use of resources (CCMC, 2014).
Source: http://www.ahrq.gov/professionals/prevention-chronic-care/improve/coordination/atlas2014/index.html
Care coordination is a process that occurs most frequently in response to transitions: across settings, across care episodes, among care providers, and as the patient’s needs change.
Case Management Goals:
- Promote patient wellness (better outcomes and increased patient satisfaction)
- Promote patient autonomy
- Manage appropriate use of services (link patient to needed services)
- Manage appropriate use of financial resources (contain cost)
Case Management Process
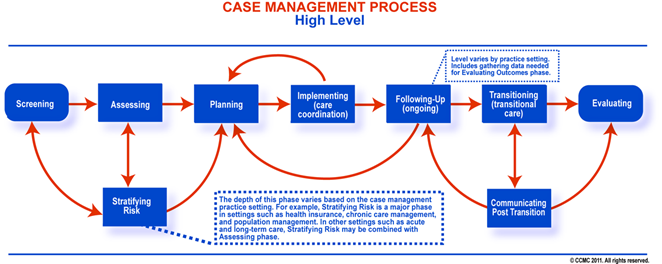
Source: https://www.cmbodyofknowledge.com/content/case-management-knowledge-2
CASE MANAGER ROLES AND RESPONSIBILITIES
The role of case manager has expanded over the years to include provider liaison, benefits interpreter, patient advocate, patient educator, triage coordinator, quality improvement, utilization, resource management, risk management, disease management, discharge planning, technology, case manager… (Finkelman, 2011).
Roles and Functions of Case Managers include:
- Assessment - conducting a comprehensive assessment of the client’s health and psychosocial needs.
- Planning - with the client, family or caregiver, the primary care provider, or other health care providers to maximize outcomes.
- Facilitating - communication and coordination between members of the health care team, involving the client in the decision making process in order to minimize fragmentation in the services.
- Advocating - for both the client and the payer to facilitate positive outcomes for the client, the health care team, and the payer. However, if a conflict arises, the needs of the client must be the priority.
(Source: CMSA Standards of Practice for Case Management, 2010).
Legal Issues in Case Management
Three conditions of liability
- Duty to provide reasonable care
- Breach of contract through an act or omission to act
- The act or omission caused injury or damage to the client
Liability for managing care:
- Failure to obtain all pertinent records on which case management actions are based
- Failure to have cases evaluated by appropriately experienced and credentialed clinicians
- Fraud and Abuse
- Making false statements of claims or causing incorrect claims to be filed
- Submitting claims for excessive, unnecessary or poor quality services
- Confidentiality/Security
- Failure to deny access to sensitive information that is awarded special protection by federal or state law
Examples of Care Coordination Models
Wagner’s Chronic Care Model is an evidence-based multifaceted approach to managing complex chronic health conditions.
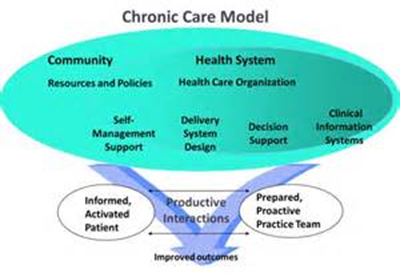
Source: https://www.act-center.org/application/files/1616/3511/6445/Model_Chronic_Care.pdf
Transitional Care Model addresses the problem of unplanned readmissions for patients with complex chronic conditions.
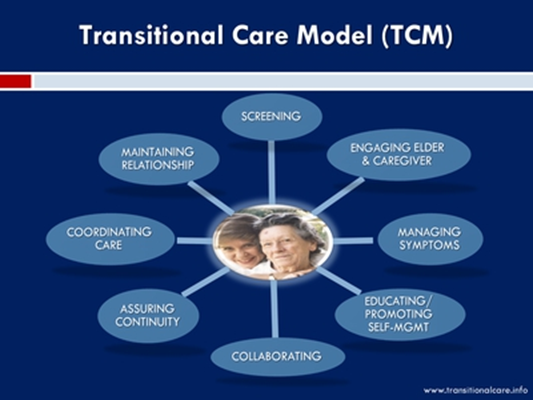
Source: https://archive.ahrq.gov/news/events/conference/2011/naylor/index.html
Transitions of Care describes “the movement of patients between health care practitioners, settings, and home as their condition and care needs change” (The Joint Commission, 2018).
Listen to the following podcast on the importance of good Transitions of Care.
Poor transitional care results in delayed diagnoses, duplicative tests, poor follow through on referrals and medication errors, costing the U.S. health system $15 billion in readmission costs and $3.5 billion in medication errors annually (National Transitions of Care Coalition (NTCC), 2012).
CASE MANAGEMENT IN THE COMMUNITY
Case Management occurs in a multitude of community practice settings; these are just a few examples:
- Ambulatory care clinics and community based organizations
- Student/university counseling and health care centers
- State and local health departments
- Public and private health insurance programs, e.g., Medicare, Medicaid, state funding programs
Where else might case management occur?
This website is maintained by the University of Maryland School of Nursing (UMSON) Office of Learning Technologies. The UMSON logo and all other contents of this website are the sole property of UMSON and may not be used for any purpose without prior written consent. Links to other websites do not constitute or imply an endorsement of those sites, their content, or their products and services. Please send comments, corrections, and link improvements to online@son.umaryland.edu.