Online Undergraduate Course
NURS 410 - Health Care Delivery Systems & Informatics
Module 11: Evaluating Health Information Technologies
Information Systems Life Cycle
WHAT IS THE INFORMATION SYSTEMS LIFE CYCLE?
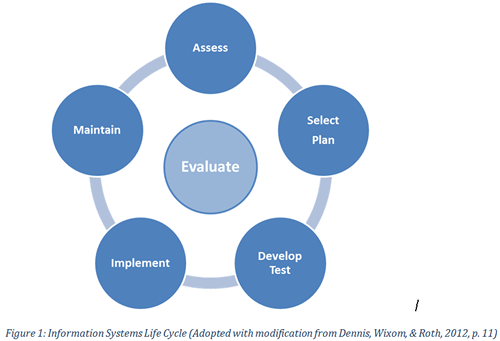
The Information Systems Life Cycle (ISLC), sometimes referred to as the systems development life cycle, is a process used to guide stages or phases of introducing or implementing new computer/information technology into an organization. There are various definitions as to the steps in this process which can range from 4 to 8 or more. Essentially, as the term “cycle” implies, the stages tend to be circular, may overlap and are repeated as needed. The ISLC is a framework often used by information technology and informatics experts but there are important implications for the clinician. For the purposes of this course we will focus on five basic stages of the Information Systems Life Cycle related to large scale projects shown in Figure 1 and how this applies to nursing. Note that evaluation occurs at each stage of the ISLC.
Stage 1: ASSESS
One of the first steps in the ISLC is not only recognizing there is a need but also whether it is possible to fix or change the issue along with identifying anticipated outcomes. Needs assessment data may be collected in a variety of ways through survey’s, observations, interviews with key stakeholders, data logged into the information technology (IT) help desk, and research studies. Informaticians will also explore current technical resources, healthcare trends, associated costs, legal/ethical issues, government or regulatory mandates as well as the impact on workflow. Usually a report is developed at this point, sometimes referred to as a “feasibility analysis”, which outlines the need (if a need actually exists), what are the gaps, limitations and possible solutions. From this data an initial scope and goals of the project may be formulated and evaluated by administrators, strategic planning committees and key stakeholders.
Role of Nursing in Stage 1
Nurses play an important role in identifying problems and deficiencies with current systems or workflow through formal and informal methods. Providing precise and well thought out explanations of issues will go a long way in identifying needs and potential solutions. Participating in surveys, interviews, workflow analysis and data flow when available provides extremely valuable information for developing a needs assessment or feasibility analysis report. Many hospitals have Nursing Information System Committees to discuss computer technology needs. These committees are familiar with organizational processes and can route system and workflow issues to informatics specialists or planning committees for consideration. Nurses should always report issues to their committee representative or the informatics specialist. In this way Nurses serve as a change agent.
Click here to learn more about feasibility studies from the business sector
Stage 2: SELECT/PLAN
At this stage a technology solution will be selected. It could be there are major issues with an existing system which may involve a system upgrade, internal programming or replacement. If a new system is needed, detailed user and technical requirements must be developed which are used to evaluate different vendor products for the best fit. Either way once a solution is identified/purchased a comprehensive plan is developed that addresses activities such as project governance, hardware and software requirements, interfaces, programming needs, user involvement, testing, training, go-live support, maintenance and more. A plan for how the system will be evaluated to determine success should also be developed at this stage. Baseline data may be collected at this point to compare with data after the new system is implemented to evaluate if there are improvements in usability, process and outcomes.
Role of Nursing in Stage 2
Nurses can assist during selection by identifying in very specific terms what they need the system to do and the anticipated impact or improvements in workflow and patient care. Organizations will solicit this information in a variety of ways through stakeholder interviews, focus groups, or surveys. Consultants may be hired to work with clinicians to formalize the details of the user requirements. Select nurses may be involved in evaluating different products for purchase or appointed to serve on various workgroups as part of the plan (more on this later). In this stage Nurses serve as a champion for practice domain needs.
Click here to view a 4-minute video about critical success factors for EHR implementations
Stage 3: DESIGN/TEST
Once a system is purchased or solution identified the plan is ready to be deployed. All solutions, whether changes to an existing system or implementing a new system, require a period of design and testing. The extent of this phase will depend on the solution. A change to an existing system may take several months to complete whereas designing a new system could take several years. This phase could involve purchase and setup of hardware to support IT infrastructure, interface design, special programming, populating database tables, designing “screens” for the user to input data into the computer, creating reports or other output, design of user training, and much, much more. If the system change has an impact on workflow, new policies or procedures may be needed.
Design and testing go hand in hand. For each change, testing must be done to ensure the system works as anticipated. There are different levels of testing that occur. IT staff will do the initial testing for bugs (coding errors) and glitches (sudden malfunction). Users may be asked to test for accuracy of the content, ease of use, satisfaction with the feature, workflow or other tasks. Testing to make sure the change works with other parts of the system or across an interface may also be done. The rule of thumb is you can never test to much so test, test, test, then test some more. Elements of design and types of testing/evaluation will be discussed more under the Human Factors section.
For large scale projects, this stage also includes developing a plan for educating care providers and other staff, creating materials, identifying teaching resources and scheduling all this within 4-6 weeks before the system is implemented. A training database has to be setup and since most systems are still being tested and redesigned up until the last minute, securing a mirror image training database of the actual system is often a moving target. Updates may be needed for users who attend training early.
Role of Nursing in Stage 3
How an information system is designed has implications for safe, efficient and effective patient care. Research supports that poorly designed systems can lead to medical errors (Karsh, Weinger, Abbott, & Wears, 2010). Although there may be informatics nurses involved in actually “designing” the system behind the scenes, the clinical nurse has a role in providing conceptual ideas and content for the design of screens and reports for data input and output related to nursing workflow. Sometimes nurses have a hard time articulating what that would look (or feel) like so paper and computer prototypes may be used as a type of iterative design process. Nurses can assist with the different levels of testing as a great way to become involved and learn how the system works. Many nurses elect to serve as system trainers or super users to assist with formal and informal user training. Nurses can also engage by providing real world clinical scenarios from their area of expertise that are used during testing and training.
Stage 4: IMPLEMENT
Another term used for implement is “go-live”. How an organization decides to do this will vary. Some choose a “big bang” approach which means all features/applications, all at once, in the entire facility. Some may deploy unit by unit or by specialty (med-surg, then pediatrics, then critical care etc.). Some may phase in by application such as CPOE first, then medication administration record, then clinical documentation and so on. Regardless of the approach there is a lot of activity just prior and immediately after the go-live date. Contingency plans are written in case things don’t work or the system crashes, user training must be done, and plans are operationalized for go-live support. Sometimes “go-live” is delayed if major issues in testing have not been resolved. For larger projects a command center may be established and available for several days or weeks after go-live to route issues back to IT for quick resolution. At this stage, the system is now live and available for users to access and incorporate into their daily workflow. The evaluation plan developed during Stage 2 will begin and continue on into stage 5 and beyond. This might include evaluating user satisfaction, utilization, turn around times or more patient focused items such as medication error rates, compliance, or specific patient outcomes.
Role of Nursing in Stage 4
Once a system or system change is implemented the nurse has a responsibility to report any issues with functionality, usability, workflow or impact on patient care. Technical issues should be reported to the IT help desk and are easier to explore if the user provides some basic information to include step by step what they were doing (options selected) from the beginning up to when the error occurred. During go-live a change in workflow is always confusing and issues may surface related to lack of familiarity with the system or new policies or procedures. Nurses can assist to clarify policies and procedures or initiate requests for system change when true workflow issues exist. Nurses designated as trainers and/or super users can provide support on their respective units or may be asked to assist with formal training of new hires.
Stage 5: MAINTAIN
Once a system is implemented and is formally accepted by the organization as passing all major requirements of the contract and users (which occurs about 60 to 120 days after go-live) we enter the maintenance phase. Clinical, technical, and business operations should be operational and somewhat routine at this point. But patient care needs often change and computer functions require ongoing updates and maintenance for optimum functioning. Procedures for routine and emergency system downtime should be effective along with a process for requesting system changes. Some organizations may have a designated nurse liaison or triage analyst to assist users in completing change requests and navigating through the process.
Role of Nursing I Stage 5
Once a system is in use for a while and an issue has not been resolved, nurses sometimes begin to ignore the problem by doing workarounds. Workarounds can be dangerous to patients if critical information is missing from their record or the technology issue goes unchecked leading to issues of data integrity. When workarounds emerge these should be discussed at the appropriate nursing committees to request system issues be re-evaluated and re-designed to enhance patient safety and workflow. Regulatory agencies sometimes require organizations to collect certain data or provide information to patients or agencies. The “meaningful use” initiative is a good example of how information systems must accommodate certain requirements related to documentation, clinical decision support and reporting. Nurses should support these initiatives and continue to be an advocate for their patients through proper use of technology.
WHAT ABOUT THE NURSING PROCESS?
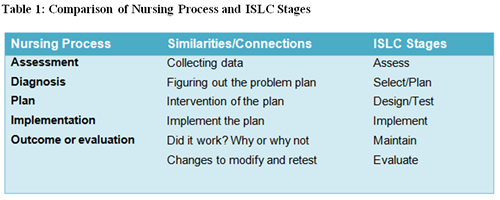
Note the similarities between the nursing process and the ISLC stages shown in Table 1
This website is maintained by the University of Maryland School of Nursing (UMSON) Office of Learning Technologies. The UMSON logo and all other contents of this website are the sole property of UMSON and may not be used for any purpose without prior written consent. Links to other websites do not constitute or imply an endorsement of those sites, their content, or their products and services. Please send comments, corrections, and link improvements to online@son.umaryland.edu.