Online Course
NRSG 780 - Health Promotion and Population Health
Module 1: Overview of Population/Public Health
Modern Era of Public Health
Two main factors have shaped our modern public health system:
- Growth of scientific knowledge
- Growth of public acceptance of disease control as both a possibility and a public responsibility
Throughout recorded history, major outbreaks or epidemics such as the plague, cholera and smallpox evoked sporadic public efforts to isolate or quarantine victims in an attempt to protect citizens from becoming infected. As scientific knowledge regarding sources of contagion and means of controlling disease became more refined, public authorities expanded measures for containing specific diseases beyond quarantine to take on new tasks including sanitation, immunization, regulation, health education and personal health care.
Five Phases of Modern Era (1850- Present)
A History of the Public Health System summarizes the five phases of the modern era of public health.
Phase 1 - Miasma (1850 - 1880)
The first phase was based on the Miasma Theory - a theory based on the belief that disease originated from rotting organic matter. Although the scientific basis of disease was poorly understood, personal and environmental hygiene gained attention as keys to mitigate spread of disease and improve health.
Two early proponents of sanitation, Chadwick in England and Shattuck in the U.S., are considered to be founders of the modern era of public health. They produced landmark data-driven reports and gained both public and government attention. Their work lead western societies and later developing countries to recognize the importance of public approaches to solving or preventing health problems. For more information, view Chadwick’s and Shattuck’s reports.
Phase 2 - Bacteriology (1880 - 1920)
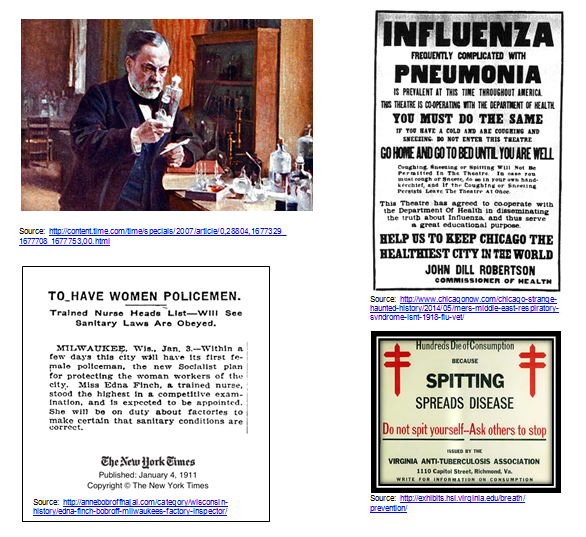
The second phase is identified as the rise of bacteriology. The work of Pasteur, Koch, and others in this rapidly growing field dramatically improved the scientific understanding of the origins of disease. During the early 20th century, many communicable diseases were checked and science became a vehicle for desired social change. The average American lifespan was extended from 47 years in 1900 to nearly 70. This shift in mortality is now termed the first public health revolution.
Despite improvement in mortality, by the 1920s it became clear that significant disability continued to exist in the 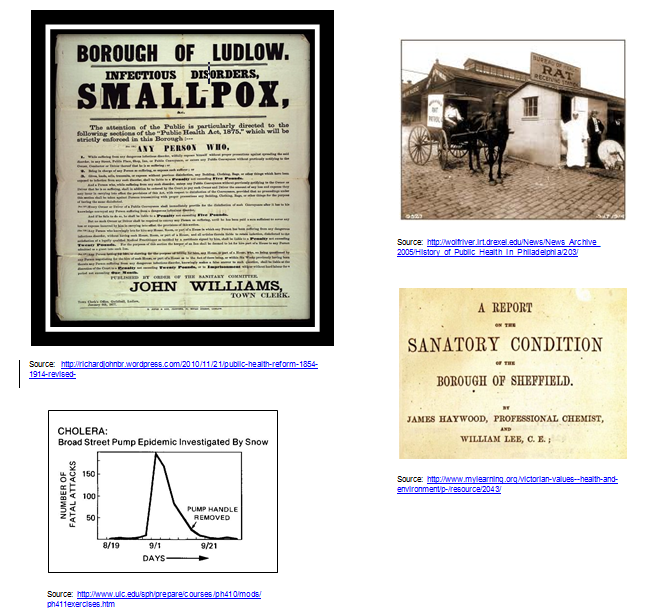 population. With the draft for WWI, 34% of young men were rejected for service due to physical or mental health disabilities. Physicians and public health experts reviewed the surprising data from the draft and recognized that while communicable diseases were well under control, other risk factors were being neglected and these resulted in chronic physical and mental health problems. Studies of disease registries and mortality and morbidity data also showed higher than expected rates of death and disability among children and the poor.
population. With the draft for WWI, 34% of young men were rejected for service due to physical or mental health disabilities. Physicians and public health experts reviewed the surprising data from the draft and recognized that while communicable diseases were well under control, other risk factors were being neglected and these resulted in chronic physical and mental health problems. Studies of disease registries and mortality and morbidity data also showed higher than expected rates of death and disability among children and the poor.
Phase 3 - Health Resources (1920 - 1960)
During the third phase, the nation believed disparities could be addressed by improving individual access to care. From 1920 to 1960 many state and county health departments established TB and child health clinics to provide medical care. Additional efforts supported health education and mass immunization programs.
Significant new funding supported hospital construction, healthcare manpower, and biomedical research and resulted in:
- establishment of the National Institutes of Health (NIH) in 1930
- passage of the Hill-Burton Act in 1947 which provided funding for hospital construction that was tied to the delivery of a percentage of free care
- increased presence of voluntary organizations like the American Heart Association (AHA)
Despite these initiatives and the proliferation of hospitals, mortality and morbidity rates did not declined significantly by 1960.
Phase 4 - Social Engineering (1960 - 1975)
During the fourth phase, leading health authorities attributed the lack of improvement in morbidity and mortality rates by 1960 to the fact that medical resources were still inaccessible to many, particularly the poor, elderly, and isolated populations. From 1960 to 1975, the nation targeted social engineering strategies to provide services to populations identified as high risk.
The Social Security Amendments of 1965, PL 89-97, 79 Stat. 286, enacted July 30, 1965, resulted in the creation of Medicare and Medicaid. The legislation provided federal health insurance for the elderly (over 65) and for poor families. Click here to watch President Johnson sign the bill into law. Additional outreach services were designed to serve groups including immigrants, Native American, and migrant workers.
As in previous periods, despite strategies to improve resource allocation and access to services, dramatic changes in morbidity and mortality did not occur. Rates of heart disease, cancer and stroke, the 3 leading causes of death, followed by accidents, COPD, cirrhosis, suicide, and homicide did not change appreciably. What did change was the per capita cost of health care.

Phase 5 - Health Promotion (1975 - Present)
By the mid-1970s, developing new approaches to preventing premature death (before age 75) became a priority.
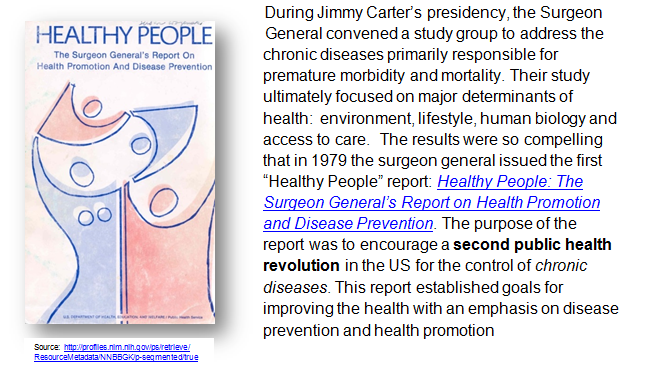
https://profiles.nlm.nih.gov/spotlight/nn/catalog/nlm:nlmuid-101584932X92-doc
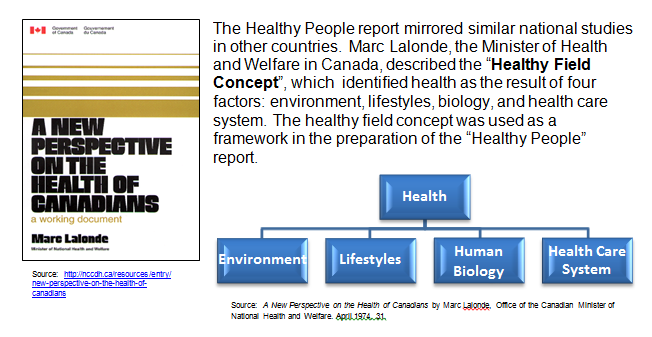
These landmark reports concluded that health is largely attributable to the four factors in approximate percentages as noted below.
| Environmental | Lifestyle | Human Biology | Health Care System | |
|---|---|---|---|---|
| Percentage | 20% | 50% | 20% | 10% |
| Examples of factors |
|
|
|
|
| Perspective | Communities can exert tremendous influence over these factors | Many of these factors are self-imposed risks | Little can be done to alter these factors | Heavily funded, often very late in the disease process |
Based on Healthy People, the Department of Health and Human Services (DHHS) works under the premise that further improvements in the health of Americans will not be achieved through greater health expenditures for increasing the number of medical services but through greater efforts designed to change lifestyles and the environment to promote health, reduce risk and prevent disease.
This website is maintained by the University of Maryland School of Nursing (UMSON) Office of Learning Technologies. The UMSON logo and all other contents of this website are the sole property of UMSON and may not be used for any purpose without prior written consent. Links to other websites do not constitute or imply an endorsement of those sites, their content, or their products and services. Please send comments, corrections, and link improvements to nrsonline@umaryland.edu.