Online Course
NDNP 804 - Theory for Evidence-Based Practice
Module 8: Theory, Model or Framework Identification
Quality Improvement Models
If you are planning on implementing a quality improvement project or study, you may want to review QI models. QI models, either alone or in combination, may be an effective approach for defining processes to be improved, identifying changes that have been effective, or guiding different approaches to changes. While it is not essential to understand all of the QI models listed in this module, a thorough understanding of several models ensures a more versatile approach to QI. Each QI model and method offers a systematic approach for assessing and improving care services.
Some quality improvement models to consider include are:
- MAP-IT
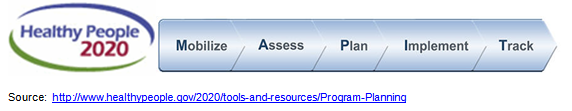
MAP-IT has five steps:- Mobilize individuals and organizations that care about the health of your community into a coalition.
- Assess the areas of greatest need in your community, and the strengths and resources that you can tap into to address those areas.
- Plan your approach: start with a vision of where you want to be as a community; add strategies and action steps to help achieve that vision.
- Implement your plan using concrete action steps that can be monitored and will make a difference.
- Track your progress over time.
How do you use MAP-IT?
- Mobilize
- Consider what you want coalition partners to do and how the coalition might be organized
- Brainstorm potential partners
- Recruit coalition members
- Create a vision for the coalition
- Assess
- Collect locally available data about resources and needs
- Collect information from public and archival sources.
- Determine what issues are most important to community residents and key stakeholders
- Identify community assets, including people, skills, capacity and capacity building, space, organizations and institutions, knowledge, funds, etc.
- Based on data and community priorities, prioritize needs by consensus
- Establish baseline data
- Plan
- Choose the issue(s) the initiative will work on
- Set clear objectives
- For each objective, develop an action plan that includes:
- A strategy and tactics
- A timeline with reasonable time targets for each phase of the strategy
- The responsible parties and their roles and tasks
- Indicators and/or other measures of progress
- Implement
- Identify an individual or organization to serve as the coordinating point for the implementation of the initiative.
- Make sure that everyone involved knows what’s going on and what everyone else is doing
- Use the media and other channels to inform the community about the work of the initiative
- Track
- Start your evaluation and monitoring at the very beginning of your initiative, if possible
- Set up a system for gathering data
- Consider:
- Data Quality
- Limitations of self-reported data
- Data validity and reliability
- Data availability
- Organize and analyze data on a regular basis, so that you can make appropriate adjustments in your work as time goes on
- Share progress and successes with the community
- Six Sigma: The model is a data-based strategy for reducing problems and improving process. This is accomplished through the use of two Six Sigma models: DMAIC and DMADV.
- DMAIC (define, measure, analyze, improve, control) is an improvement system for existing processes falling below specification and looking for incremental improvement.
- DMADV (define, measure, analyze, design, verify) is an improvement system used to develop new processor products at Six Sigma quality levels.
Aveta Business Institute. (n.d.) The Six Sigma models and their uses. Retrieved from http://www.sixsigmaonline.org/six-sigma-training-certification-information/the-six-sigma-models-and-their-uses/

Source: http://sixsigmatraining.page.tl/
- Plan-Do-Study Act (PDSA): The model is most commonly used method in health care for rapid cycle improvement, also called Deming Cycle. It is a trial-and-learning approach or action-oriented learning where a hypothesis is made and tested on small scale before any changes are made to the system. The model tests a change by planning it, trying it, observing the results, and acting on what is learned. The steps in the PDSA cycle are:
- Step 1: Plan
- Plan the test or observation, including a plan for collecting data
- State the objective of the test.
- Make predictions about what will happen and why.
- Develop a plan to test the change. (Who? What? When? Where? What data need to be collected?)
- Step 2: Do
- Try out the test on a small scale.
- Carry out the test.
- Document problems and unexpected observations.
- Begin analysis of the data.
- Step 3: Study
- Set aside time to analyze the data and study the results.
- Complete the analysis of the data.
- Compare the data to your predictions.
- Summarize and reflect on what was learned.
- Step 4: Act
- Refine the change, based on what was learned from the test.
- Determine what modifications should be made.
- Prepare a plan for the next test.
Institute for Healthcare Improvement. (2016). How to improve. Retrieved from http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx
- Knowledge to Action (KTA) Framework
The KTA framework is designed to facilitate knowledge translation through an iterative, multifaceted and dynamic process that enables a deliberate change in practice. The framework includes three phases of knowledge creation: knowledge inquiry, knowledge synthesis, and development of knowledge tools (i.e., practice guidelines, decision-aides or algorithms). Graham and Tetroe (2010) describe this process as a sieve, filtering knowledge in order to make the results more informative for the targeted audience. The KTA framework also incorporates seven action stages:- identify a problem
- adapt knowledge to the local context
- assess facilitators and barriers to knowledge use
- select, tailor and implement intervention
- monitor knowledge use
- evaluate outcomes
- sustain knowledge use
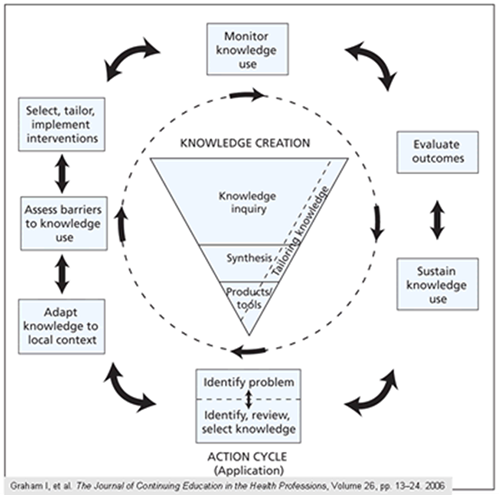
These action stages can occur consecutively or concurrently and all can influence the knowledge creation phase of the framework.
Reference:
Graham, I. D., & Tetroe, J. M. (2010). The knowledge to action framework. In J. Rycroft-Malone & T. Bucknall (Eds.), Models and frameworks for implementing evidence-based practice: Linking evidence to action (pp. 207-222). Oxford: Wiley-Blackwell
- Promoting Action on Research Implementation in Health Services (PARISH) Framework
The PARIHS framework has three key elements: the nature of the evidence, the quality of the context of implementation, and appropriate approaches to facilitation. Evidence is described as sources of knowledge as perceived by multiple stakeholders. Context describes the quality of the environment where the project is being implemented. Facilitation is a technique to support others to change in attitude and skills. The success of implementing evidence-based practice and the sustainability of the innovation is dependent upon the strength and appropriateness of these key elements.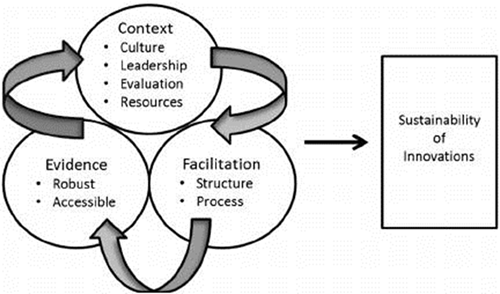
Reference:
Rycroft-Malone, J. (2010). Promoting on Research Implementation in Health Services (PARISH). In J. Rycroft-Malone & T. Bucknall (Eds.), Models and frameworks for implementing evidence-based practice: Linking evidence to action (pp. 109-136). Oxford: Wiley-Blackwell.
This website is maintained by the University of Maryland School of Nursing (UMSON) Office of Learning Technologies. The UMSON logo and all other contents of this website are the sole property of UMSON and may not be used for any purpose without prior written consent. Links to other websites do not constitute or imply an endorsement of those sites, their content, or their products and services. Please send comments, corrections, and link improvements to nrsonline@umaryland.edu.