Online Course
NRSG 780 - Health Promotion and Population Health
Module 4: Primary, Secondary, and Tertiary Prevention
Levels of Prevention
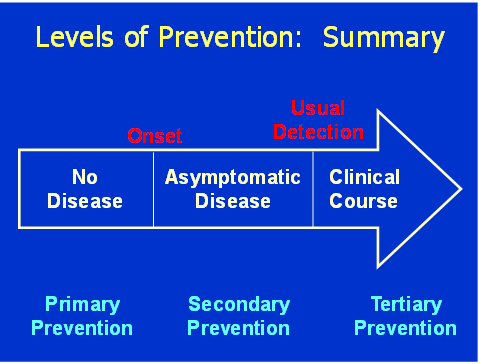
There are three levels of prevention: primary, secondary and tertiary.
Primary Prevention
Primary prevention describes interventions aimed at preventing occurrences of disease, injury or disability. Primary prevention strategies focus on a population the does not have a disease that an initiative is trying to prevent.
Immunizations are a familiar example of primary prevention. As a society, we have been very concerned about vaccine-preventable diseases.
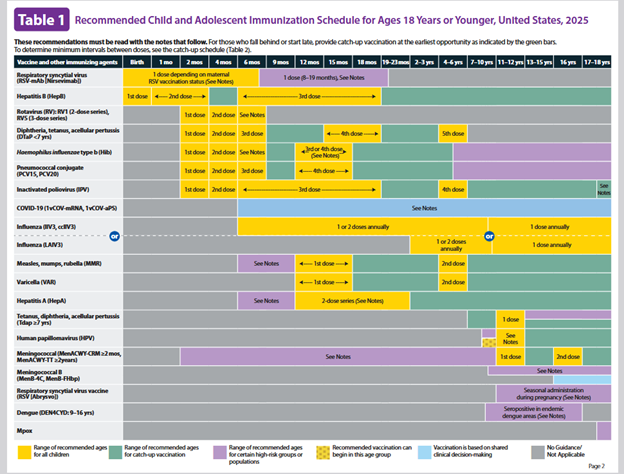
Source: https://www.cdc.gov/vaccines/schedules/downloads/child/0-18yrs-child-combined-schedule.pdf
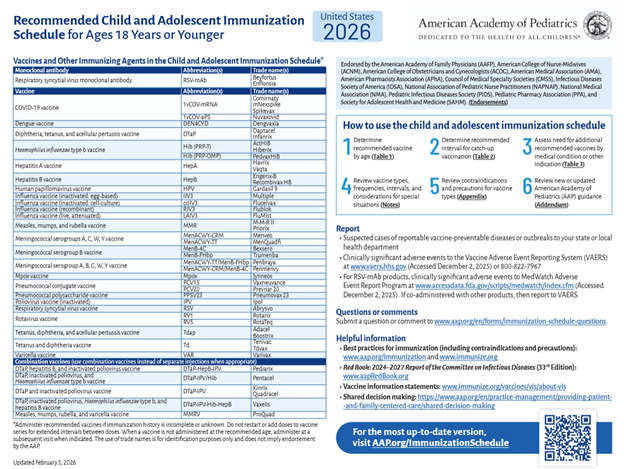
In January 2026, the US Department of Health and Human Services modified the recommendations for childhood immunizations reducing the number of recommended vaccines from 17 to 10 based on international consensus as well as varicella (chickenpox). For more information review the fact sheet at https://www.hhs.gov/press-room/fact-sheet-cdc-childhood-immunization-recommendations.html. By the end of January the American Academy of Pediatrics issued its own recommended schedule endorsed by twelve professional societies and differs from the new CDC immunization schedule. For more information review https://www.aap.org/en/patient-care/immunizations/
Pediatric and family practitioners and many parents recognize the importance of and follow the vaccine schedules for children. Proof of immunizations is required by many institutions, such as day care, schools and health care settings. This requirement further reinforces this primary prevention measure.
Another example of primary prevention is exercise. Let's Move! was an initiative, launched by the former First Lady, that provides parents with helpful information to help children become more physically active, eat a healthy diet and maintain ideal weight.
Not starting smoking or early smoking cessation are also primary prevention strategies geared toward preventing heart disease, cancer, stroke and many other diseases.
Secondary Prevention
Secondary prevention describes initiatives aimed at early detection and treatment of disease before signs and symptoms occur. Secondary prevention focuses on the population that has disease, but in its earliest stage. With early detection and intervention, secondary prevention strategies can be effective and significantly enhance health care outcomes.
Secondary prevention is often equated with screening, but it is actually broader than screening alone and includes early intervention.
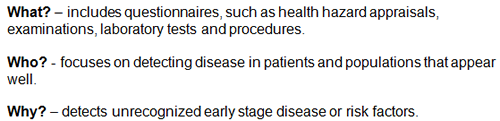
Screening is defined in terms of What, Who and Why.
Population screening is not appropriate for all diseases. Screenings should focus on important health problems that result in significant morbidity and mortality for the population as a whole. This would include:
- diseases with a high incidence or prevalence rates
- disabilities that significantly decrease quality of life
- diseases that have a high mortality rate.
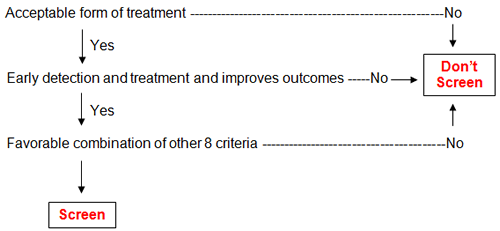
Criteria for screening include:
- an important health problem
- an acceptable form of treatment
- evidence that early detection and treatment improves the outcome
- an understanding of the natural history of the disease
- a recognizable latent stage
- a suitable screening test
- availability of diagnostic/treatment facilities
- an agreed upon policy on whom to treat
- a reasonable cost of screening
If there is not an acceptable form or treatment, or early detection/treatment does not improve the outcomes, or few of the other criteria are met, then screening may be inappropriate.
Successful screening programs are:
- Valid (accurate)—High probability of correct classification of person tested
- Reliable (precise)—Results consistent from place to place, time to time, person to person
- Capable of large group administration—Fast and inexpensive
- Innocuous—Minimally invasive and few side effects
- High yield—Ability to detect enough new cases to warrant the effort and expense
Validity is measured by sensitivity and specificity. Commit the definitions below to memory:
- Sensitivity measures the proportion of persons with the disease correctly identified as positive (true positives)
- Specificity measures the proportion of persons the test correctly identifies as negative for the disease (true negatives)
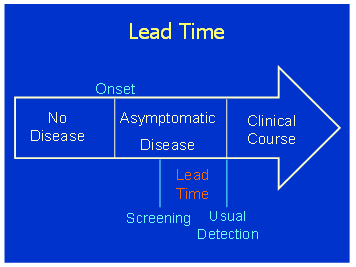
Screening is appropriate when there is a significant latent phase and detecting the problem early will lead to improved outcomes and improved survival.
Evaluation of a Screening Program - screening programs are considered effective when they:
- reduce the burden of disease
- enhance quality of life
- reduce mortality rates.
| Examples of Good Screening Tests* | Examples of Bad Screening Tests |
|---|---|
| Questions about lifestyle risk factors (e.g., diet, smoking, physical activity) | Chest X-ray |
| Dental exam | Resting EKG |
| Pap smear | Exercise EKG |
| Blood pressure measurement | Urinalysis |
| Screening for osteoporosis in the ≥ 60 years of age | PSA |
| Skin examination | CBC |
| Blood cholesterol measurement | Thyroid function tests |
| Stool hemoccult | |
| Sigmoidoscopy/colonoscopy ≥ 50 years of age | |
| Mammography for women ≥ 50 years of age | |
| Blood lead levels (in high-risk populations) | |
| Metabolic diseases of childhood (e.g., PKU hypothyroidism) |
*not all of these are appropriate for community screening settings
Tertiary Prevention
Tertiary Prevention includes interventions aimed at preventing further morbidity, limiting disability and avoiding mortality and interventions aimed at rehabilitation from disease, injury or disability.
Examples: insulin for diabetes, penicillin for pneumococcal pneumonia, CVD exercise programs, drug therapy, substance abuse treatment programs.
Summary: This schematic may help in summarizing primary, secondary and tertiary prevention in relation to disease onset and usual detection.
This website is maintained by the University of Maryland School of Nursing (UMSON) Office of Learning Technologies. The UMSON logo and all other contents of this website are the sole property of UMSON and may not be used for any purpose without prior written consent. Links to other websites do not constitute or imply an endorsement of those sites, their content, or their products and services. Please send comments, corrections, and link improvements to nrsonline@umaryland.edu.