Online Course
NDNP 819: Advanced Health Assessment Across the Lifespan
Module: Peripheral Vascular and Lymphatic System
Abdomen
History Components
A focused history always helps the APRN to narrow in on a working differential diagnosis. To help you with the abdomen you need to think about the location of the pain, the type of pain, the associated symptoms and the age and sex of your patient as this information guides your history and ROS. Your ROS questions for a 45 year-old male presenting with c/o abdominal pain are different from a 45 year-old female. Remember that cardiac, pulmonary and genitourinary problems can manifest as abdominal symptoms so be prepared to also ask a history and ROS of these systems also.
Location review: https://meded.ucsd.edu/clinicalmed/abdomen.htm
This website is a good review of locations of abdomen and great pictures of abnormal findings as well.
Types of Abdominal Pain:
Visceral Pain: Visceral pain is directly related to the organ involved and the majority of organs do not have an abundance of nerve fibers. Visceral pain is less severe and poorly localized. This does not mean the patient is experiencing a mild or less severe condition. The pain is usually dull or aching and constant or intermittent.
Parietal Pain: Parietal pain occurs when there is an irritation of the peritoneal lining. The peritoneum has a higher number of sensitive nerve fibers, so the pain is generally more severe and easier to localize. Pain is usually sharp, constant and on one side or the other.
Referred Pain: Referred pain is visceral pain that is felt in another area of the body and occurs when organs share a common nerve pathway. It is poorly localized and generally constant in nature. An example is a patient with liver problems that experiences referred pain in the neck or just below the right scapula.
Past Medical History: Has the patient ever been told or diagnosed with: urinary tract infection, pyelonephritis, appendicitis, liver or gallbladder disease, hepatitis, pancreatitis, inflammatory bowel disease (Crohn’s or ulcerative colitis), Irritable Bowel Disease, Colon CA, Peptic ulcer disease, GERD, MI, PE or AAA?
Any history of ectopic pregnancy, ovarian cyst or cancer and endometriosis in a female patient versus testicular torsion or prostate cancer in a male patient? Here are some examples in variations of history taking that would be important to include depending on age group.
- Infant: History of growth, development and immunizations. History of colic, vomiting, poor feedings with fussiness?
- Child: History of appendicitis or constipation?
- Teen: Diet history is important here: Any irregular patterns of eating?
- Pregnancy: Any history of nausea, vomiting, constipation or reflux?
Surgical History: Has the patient ever had abdominal surgery such as appendectomy, cholecystectomy, C-section, hernia repair, urethral stents, prostate?
Family Medical History: Does the patient know if their parents, siblings or grandparents had any of the following conditions? Colon CA, Celiac disease, Inflammatory disease, ovarian cancer, prostate CA? These are red flag conditions due to their strong familial/genetic component.
Social History: Any history of alcohol, tobacco, other smoking or drugs including IV drug use (hepatitis) and drugs not prescribed for them?
Diet/Elimination/Sleep/Immunizations: Think about age of patient here as the questions vary considerably.
- Diet of an infant or child: bottle or breast fed, table foods, how much and how often? Any spitting up? Teens: ask about activity or any recent weight gain or loss. Ask about a 24-hour diet history including beverages. For the older adult, how do they get their groceries and prepare food? Do they get up at night to urinate or have problems with constipation?
- When and what were their last immunizations? Have they been vaccinated for Hepatitis A and/or B?
Review of Systems: These systems need to be included and think about how they change for the following populations: Infants, Children and Teens, Adults and geriatrics and pregnancy.
- General: wt. gain or loss, skin color changes, fatigue
- Skin: yellowing of skin or eyes
- CV & Pulm: chest pain, SOB
- GI: last colonoscopy? Ever had an endoscopy? N/V/D/C. In pregnancy more incidence of constipation and acid reflux r/t decrease GI motility.
- GU: LMP, STI history, pregnancy history, urinary symptoms (different for male vs. female)
Physical Exam
The order of the abdominal exam is: inspection, auscultation, palpation and percussion. Please watch this video for an example of an abdominal exam.
Abdominal Exam Techniques:
- Provide privacy, good lighting/appropriate temp in room, expose the abdomen, empty bladder, position pt supine, arms by side & head on pillow with knees slightly bent or on a pillow
- Warm stethoscope & hands
- Painful areas last with distraction techniques
Inspection: Note shape (flat, scaphoid, rounded protuberant), venous patterns, bulges, scars, lesions or striae, movement of abdominal wall with respiration with children
Auscultation: Don’t forget to auscultate before percussing! Use diaphragm and press lightly. What do you hear? Hypoactive, Hyperactive, Normoactive (5-34 per minute), or Absent (2 or more minutes). Other sounds: Borborygmi (a rumble or prolonged gurgles) Tinkles (high pitched ‘drips’ heard in dilated bowels with air fluid).
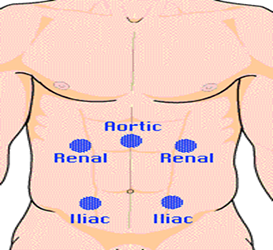
Use bell for vessels: Here is a diagram for arteries to auscultate. What do you hear? Atherosclerois may alter arterial blood flow so that a bruit is heard.
Percussion: General quadrants and organs. Why and how do we percuss? Detect fluid, gaseous distention and masses. Gently tapping on the skin to create a vibration
- Tympany- gas (dominant sound because of air in sm intestine). Normally all quadrants should be tympanic (hollow-like drum)
- Dullness- solid masses, distended bladder, enlarged liver or spleen or tumor
- Percuss liver, spleen, kidneys
Liver Span
- Percuss downward from the chest in the right mid-clavicular line until you detect the top edge of the liver dullness
- Percuss upward from the abdomen in the same line until you detect the bottom edge of liver dullness
- Measure the distance between these two points (normal is 6-12 centimeters)

Assessing for Splenic Dullness
- Percuss the lower costal inter-space in the left anterior axillary line
- Ask the patient to take a deep breath and hold it while you percuss again
- This area is normally tympanic
- Dullness suggests splenic enlargement
Palpation: Light and Deep
- Watch pt. face for any grimacing or sign of pain or discomfort.
- Always inspect skin for lesions, rash, striae, masses, turgor or moles.
- Use one hand for light palpation and two hands for deep. Keep fingers together and lift hand moving to next area of abdomen without jumping over an area. Go Clockwise starting in RUQ or in area without pain first.
Ticklish or anxious patients may do better when you use their hand to palpate these areas first
Palpate the liver: stand on the right side of pt. take a deep breath in and while they let out press inwards and upwards of the RUQ to note any enlargement or tenderness (Murphy Sign).
Palpate the spleen: remain on patient’s right side, reach across with the left hand placing it under the left CVA and use right hand to gently press inward to the left costal margin while the pt. takes a deep breath. The spleen should not be palpable. It is a normal finding to not feel an enlargement of the spleen.

Video Examples of Special Tests for the Abdomen. Please review.
This website is maintained by the University of Maryland School of Nursing (UMSON) Office of Learning Technologies. The UMSON logo and all other contents of this website are the sole property of UMSON and may not be used for any purpose without prior written consent. Links to other websites do not constitute or imply an endorsement of those sites, their content, or their products and services. Please send comments, corrections, and link improvements to nrsonline@umaryland.edu.